Formation Of Periventricular Cysts In Periventricular Leukomalacia And Brain Injury At Birth
The medical malpractice attorneys at Hixson & Brown have represented numerous families whose baby’s or infants have suffered a brain injury at birth; either during labor or delivery. Such brain injuries can include periventricular leukomalacia, hypoxic ischemic encephalopathy and cystic encephalomalacia. In most of these cases, the timing of the brain injury has been an issue. The defendant hospital, physicians or nurses usually attempt to assert that the brain injury occurred during gestation and well before birth. This is an attempt to assert that the periventricular leukomalacia, hypoxic ischemic encephalopathy or cystic encephalomalacia were not the result of any negligence on the part of the medical care providers. The formation of cystic structures in the brain can help identify the approximate timing of the brain injury.
When a hypoxic event during gestation, labor or delivery is significant, areas of the baby’s brain can die (become ischemic) due to the lack of oxygen. If this occurs, the dead brain tissue is reabsorbed by the body leaving what appears to be a hole in the brain. These holes are referred to as cysts or cystic structures.
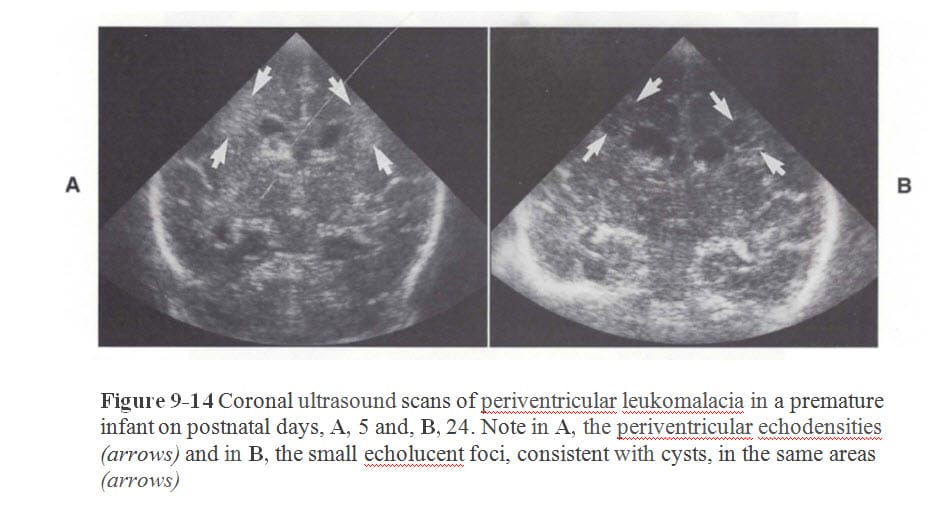
Since medical science has studied the formation and timing of these cystic structures, the appearance of the cysts on brain imaging (ie: ultrasound, MRI or brain CT) can be used in part to time the injury. Cystic structures can be seen from the images below contained in J. Volpe, Neurology of the Newborn – 4th edition, p. 344 (2001):
If a baby with severe brain injury has an ultrasound on day of life #1 which shows extensive cysts throughout the white matter of the brain, it is more likely than not the brain injury occurred at least a week prior to birth. However, if the brain ultrasound is not done until 13th day of life, the timing of the brain injury and cystic changes become more difficult. This is because the defendant hospital, physicians and nurses may claim that brain cysts take at least 2-3 weeks to form. Thus, the argument is that if the cysts were present on brain imaging at 13th day of life, then they must have preceded birth by at least one day. Although such an argument by the defendants in a medical malpractice case may have some support in the medical literature, a closer look shows the argument to lack merit in some cases.
The medical malpractice lawyers at Hixson & Brown had a case similar to the above scenario. After significant research and work with medical experts, the medical malpractice attorneys were able to show that the two to three week window for the formation of brain cysts in a 32 week premature baby who suffered from periventricular leukomalacia and multicystic encephalomalacia was not applicable.
An excerpt from the report of a pediatric neuroradiologist hired by the medical malpractice lawyers provided the following:
Baby’s imaging does reveal multicystic encephalomalacia. Such an injury is usually the result of postnatal events as reflected in the following excerpt:
Multicystic encephalomalacia is usually the result of postnatal hypoxic-ischemic events and is uncommonly seen at birth (Fig. 14.3). Etiology of this entity is more diverse than in porencephaly or hydranencephaly and may be due to vascular, watershed, infective or metabolic diseases.
There is increasing evidence that hypoxic-ischemic lesions considered typical for peri and postnatal injury, such as PVL, multicystic encephalomalacia, or even parasagittal cerebral injury, can occur in utero, usually late in gestation, that is, in the second part of the third trimester (Table 14.6).
Neuroimaging Clinical and Physical Principles, RA Zimmerman, 2000, p. 535. Baby was at 31 4/7 weeks gestation and had not reached “the second part of the third trimester.” Thus, the multicystic encephalomalacia and PVL that baby suffers from “is usually (more likely than not) the result of postnatal hypoxic-ischemic events.”
As noted above, baby’s initial ultrasound on 13th day of life revealed evidence of multicystic encephalomalacia. Multicystic injuries such as this are normally caused by perinatal or postnatal events as shown by the following excerpt:
Pathology And Imaging Features
Imaging of intrauterine ischemic insults is characterized by defects in the brain substance that can cross the entire hemisphere, may communicate with the ventricle, and may be closed or open. The defect can also have a more cystic appearance, with a single cyst or multiple cystic cavities or cystic transformation of most of the cerebral hemispheres. Closed or open acquired clefts are hallmarks of early or later lesions acquired in utero. This is also true for cystic “replacement” of infarcted hemispheric substance in hydranencephaly or basket brain. If similar extensive lesions are caused by peri or postnatal events, they are more likely to be multicystic and have a very noticeable, dramatic or iatrogenic clinical background.
Id. at 537. As indicated, “closed or open acquired clefts are hallmarks of early or later lesions acquired in utero.” Baby did not have evidence of this on his brain imaging. As I testified during my deposition, I believe the imaging shows an event occurring around the time of birth or in the immediate postnatal period. The above excerpt supports my opinion.
The Baby’s Head US Revealed:
Multiple coronal and sagittal images of the brain show normal ventricular size, outline and position. However, there were multiple periventricular cysts of various sizes around the ventricular outline. In addition, there is an additional cyst measuring 1.25 x 1.45 cm, contiguous and posterior to the right occipital horn.
“A solely prenatal PVL tends to have a more frontal and fewer occipital involvement.” The following excerpt is from Chapter 14 and supports my opinion:
Congenital Hypoxic-Ischemic Lesions With Atypical Peri or Postnatal Pattern
Hypoxic-ischemic lesions that are usually associated with peri- or postnatal injury may be acquired in utero well before birth. Classic territorial infarction, periventricular leukomalacia (PVL), multicystic encephalomalacia, or laminar cortical necrosis have been observed in stillborn infants, monozygotic twins, and in newborn infants, with full development of lesions at birth. The recognition and documentation of these lesions at birth can give clear evidence of their prenatal nature. High resolution, high quality ultrasonography (7MHz probe) can detect and identify many of these lesions in newborn infants, although MRI might reveal additional relevant information. A solely prenatal PVL tends to have a more frontal and fewer occipital involvement and fewer spastic deficits than a comparable peri or postnatal PVL.
Id. at 538. Baby’s brain imaging did not reveal the “more frontal … involvement” that you would expect from a “solely prenatal PVL.”
Counsel for the defendants also asked me about the timing of the cystic structures that could be seen in baby’s brain imaging. I informed him that it takes about 10 days to see cystic changes in the white matter. When asked about any literature that may support my opinion on timing, I directed defense counsel to Chapter 14 in Neuroimaging Clinical and Physical Principles. I have set forth below some excerpts from Chapter 14 that support my opinion on timing.
First, the table below deals with imaging correlation in the wake of hemorrhage. Although baby did not suffer a hemorrhage, the timing of evolution to echolucency (cysts) would be the same. The below table shows that an “echolucent center” (a cyst) would have an “estimated age” of “one or more weeks.”
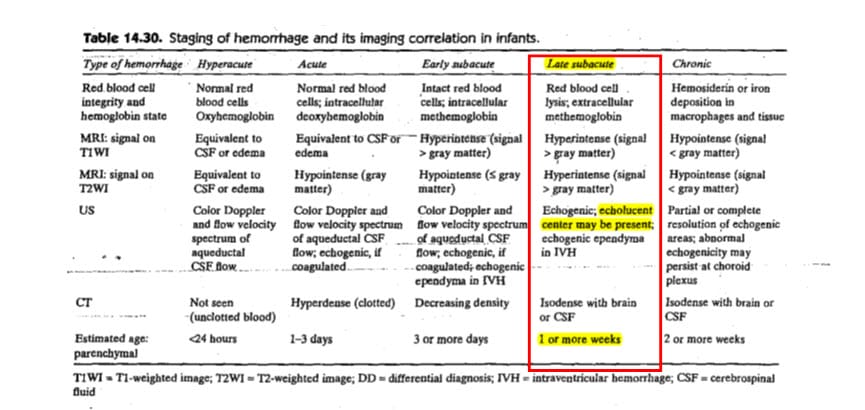
Id. at 573. This would be consistent with my opinions in the case.
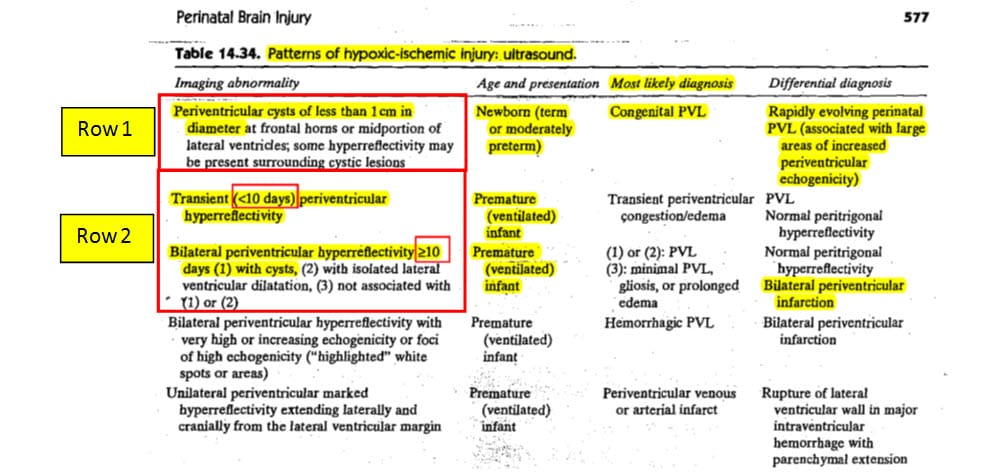
In Table 14-34 below, patterns of hypoxic-ischemic brain injury and their appearance on ultrasound are discussed. In what I have labeled “Row 1”, you can see a description for PVL related cysts “of less than one centimetre in diameter at frontal horns” in the term or moderately preterm infant. As discussed above, when there is a “frontal” predominance and the infants are in the “2nd part of the 3rd trimester” or later, the most likely cause would be “congenital.” This does not apply to the baby in this case because he had a more posterior predominance and, as noted above, he was not yet in the 2nd part of the 3rd trimester. Thus, his injury is, in all probability, not congenital. In “Row 2”, you will find ultrasound findings related specifically to “premature (ventilated) infants” like the brain injured baby in this case. When the ultrasound findings reveal “bilateral periventricular hyperreflectivity ≥ 10 days with cysts”, the “most likely diagnosis” is periventricular leukomalacia (PVL). This supports my testimony that cystic structures in premature ventilated babies like the baby in this case can be seen as early as “10 days” after an acute insult.
My testimony on the timing of these cystic structures is also supported by Joseph Volpe in his well-recognized publication: Neurology of the Newborn. In the 4th Edition (2001), Volpe provides:
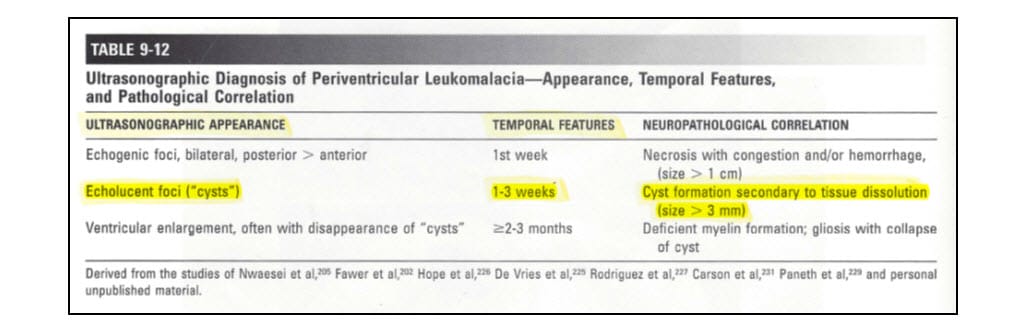
J. Volpe, Neurology of the Newborn – 4th edition, p. 344 (2001). Volpe then goes on the state:
The evolution of the ultrasonographic appearance of focal periventricular leukomalacia has been defined clearly by studies reported by others and by approximately 20 years of personal experience with this imaging technique (Table 9-12). In coronal projections, the acute lesions appear on sonograms as bilateral, often linear or “flare” echo densities adjacent to the external angles of the lateral ventricles (Fig. 9-14). In coronal projections angled slightly posteriorly, the echo genic lesions are visualized better because the peritrigonal region is imaged (Fig. 9-15). On parasagittal projections, the echodensities may be diffusely distributed in periventricular white matter or localized to the sites of predilection for periventricular leukomalacia, i.e., the regions adjacent to the trigone of the lateral ventricles or to the frontal horns at the level of the formina of Monro, particularly the former, or both (Fig. 9-16) (see Chapter 8). The characteristic evolution of the echo densities of periventricular Leukomalacia is the formation of multiple small echolucent cysts, sometimes rendering a “Swiss cheese” appearance (Figs. 9-15 and 9-16), after approximately 1 to 3 weeks.
Id. at 344. As you can see, Volpe reports that cysts can be seen after approximately one to three weeks. In his 5th Edition of Neurology of the Newborn, Volpe provides:
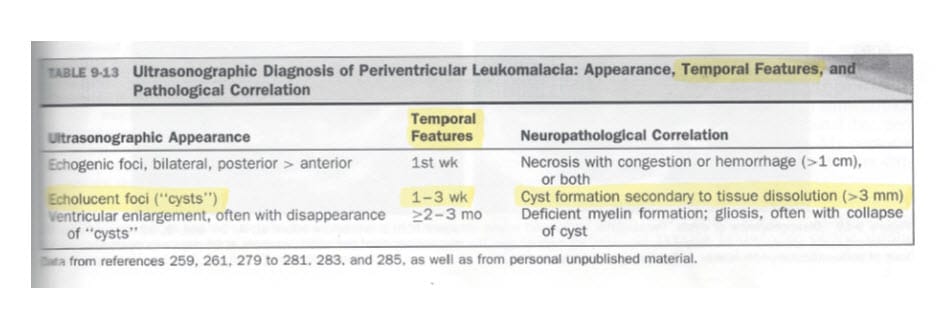
J. Volpe, Neurology of the Newborn – 5th edition, p. 417 (2008). Volpe’s 5th Edition also supports my opinions on timing of cystic formations to be between one and three weeks in this case.
In addition to the above medical text books, in 2001, prior to baby being born, T. Kubota, et al., specifically studied the relationship between cyst formation seen on ultrasound and the timing of injury in preterm infants with PVL. See, T. Kubota, Relationship Between The Date Of Cyst Formation Observable On Ultrasound And The Timing Of Injury Determined By Serial Electroencephalography In Preterm Infants With Periventricular Leukomalacia, Brain & Development 23: 390-394 (2001). I have attached a copy of this article to this report for your review. Some parts of the article are worth pointing out. On page 392, Kubota reports on a preterm infant (24 weeks) who had no evidence of cystic structures at birth and a known postnatal injury at 35 days of age. The date of cystic structure formation was 46 days of age with an “estimated interval between the brain insult and cyst formation [of] 11 days.” Here is the excerpt for your convenience:
One infant with a presumed postnatal injury (gestational age, 24 weeks; birth weight, 730 g) experienced cardiac arrest due to severe hyperkalemia of unknown origin at 35 days of age. EEGs before this event were normal, but an EEG at 39 days of age revealed both acute and chronic stage EEG abnormalities. We consider that cardiac arrest due to hyperkalemia was responsible for the brain injury in this infant. The date of cyst formation was 46 days of age. Therefore, the estimated interval between the brain insult and cyst formation was 11 days.
Id. at 392. Kubota also found that when the cysts were widespread, as in this baby’s case, the temporal range of cyst formation was between 10 – 27 days:
The median date of cyst formation was 23 days (range, 16- 39 days) in nine infants with localized cysts and 15.5 days (range, 10-27 days) in 18 infants with widespread cysts. The date of cyst formation was significantly earlier in the infants with widespread cysts than in those with localized cysts (Fig. 4; P , 0:01).
Id. at 392. Lastly, Kubota found that the severity of the insult had an effect on the timing of cystic formation:
The date of cyst formation was remarkably earlier in infants with widespread cysts, i.e. more severely affected infants, than in those with localized cysts. It is well known that the severity of neurological sequelae is correlated with the extent of cyst formation in infants with PVL. This suggests that the date of cyst formation will be largely dependent on the severity of PVL. The severity of pathological changes may also parallel that of ultrasonographic findings. It can be presumed that the more severe the degree of PVL, the earlier the cyst will reach the threshold size for ultrasonography.
Id. at 393. This baby had clinically significant postnatal events that are well recognized as being associated with or causing periventricular leukomalacia in preterm infants.
Based on the above, it remains my opinion that this baby’s injuries, as reflected in the brain imaging studies, are most consistent with an injury occurring around the time of his birth and are consistent with the Hypercarbia and hypoxic events occurring on day of life #2.
Based on the above expert report obtained by the medical malpractice attorneys at Hixson & Brown, as well as other reports obtained from other medical experts, the above case was settled prior to going to trial.
If you have a baby who suffers from Cerebral Palsy as a result of periventricular leukomalacia (PVL) or cystic encephalomalacia with evidence of cysts on ultrasound or MRI, you should obtain a copy of the medical record and the brain imaging to see if the timing of the injury indicates that the brain injury occurred during labor and deliver or due to postnatal events. You should also contact a lawyer or attorney who has expertise handling these types of medical malpractice cases.
